How to Communicate with Someone Living with Parkinson’s

Author: Home Helpers Home Care
Communication is a vital part of maintaining relationships, especially for those living with Parkinson’s disease.
As Parkinson’s progresses, it can affect speech clarity, vocal volume, and facial expressions. This makes it harder for the person with Parkinson’s to express their thoughts and emotions. These communication difficulties can be frustrating and confusing. They may also leave the person with Parkinson’s, along with their family members and caregivers, feeling isolated.
One common scenario involves asking a loved one what they would prefer for dinner. Prior to the onset of Parkinson’s, this would have been a straightforward and brief exchange. Now, with slower speech and delayed responses, it may take much longer, or the answer may never come at all. For both parties, this moment can be stressful or disheartening.
Fortunately, there are ways to make communication more manageable and less stressful.
Learning how to communicate effectively with someone living with Parkinson’s begins by adjusting your communication style. Using empathy and patience can make daily interactions more successful.
Below are detailed communication tips for Parkinson’s care. These strategies can help you create more supportive conversations, reduce stress, and promote emotional well-being for everyone involved.
Why Communication Matters in Parkinson’s Care
The Parkinson’s Foundation reports that about 89% of people with Parkinson’s have some type of speech or voice disorder. These challenges aren’t just physical, they affect confidence, independence, and social engagement.
Effective communication enhances quality of life and emotional well-being. It allows people with Parkinson’s to participate in decisions, maintain relationships, and express their needs and feelings. For caregivers, improving communication reduces misunderstandings, strengthens trust, and promotes a more positive caregiving experience.
As Parkinson’s progresses, speech difficulties can make it harder to attend doctor’s appointments or explain important symptoms. That is why it helps when caregivers speak up, so others know what the person wants, how they’re feeling, and what’s important to them.
When communication breaks down, so does trust and quality of care. Recognizing communication difficulties early allows caregivers to adjust and better support their loved one’s changing needs.
Below are detailed communication tips for Parkinson’s care that can help you create more supportive and successful conversations while promoting emotional well-being and reducing stress for everyone involved. These tips apply to all types of communication—spoken, written, visual, and even nonverbal.
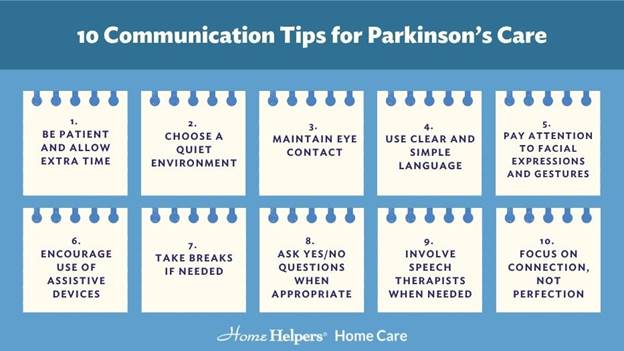
10 Communication Tips for Parkinson’s Care
1. Be Patient and Allow Extra Time
People with Parkinson’s often process thoughts more slowly and may struggle to get words out clearly. Avoid interrupting or finishing their sentences. Instead, give them ample time to speak and maintain a calm, relaxed demeanor.
Silence doesn’t mean confusion—it may simply mean they are organizing their thoughts. Your patience creates a comfortable space for open communication and helps reduce pressure or anxiety for the person with Parkinson’s.
2. Choose a Quiet Environment
Background noise can make it harder to hear or concentrate. Choose a quiet, peaceful location to have conversations. Turning off the TV, silencing phones, and minimizing distractions allows the person with Parkinson’s to focus better and feel more at ease.
A calm setting supports better hearing, clearer speech, and more successful conversations. Whenever possible, sit face to face so both parties can read each other’s expressions and gestures more easily.
3. Maintain Eye Contact
Looking someone in the eye helps build trust and connection. Since individuals with Parkinson’s may struggle with facial expressions due to facial masking, eye contact ensures you stay emotionally engaged and provides visual cues to support understanding. Maintaining gentle eye contact also shows that you are actively listening and fully present in the moment.
If the person has difficulty making eye contact, don’t worry, your effort still matters. Position yourself at eye level, gently touch their hand if appropriate, and use a calm tone of voice. These subtle, reassuring actions reinforce that you’re listening with your full attention, even if facial expressions are harder to interpret.
4. Use Clear and Simple Language
Avoid long or complicated sentences. Speak slowly, enunciate clearly, and use straightforward language. Breaking complex ideas into smaller pieces can also help. This makes it easier for someone with cognitive symptoms to follow along and respond appropriately.
Repeating keywords or rephrasing when needed can also help reinforce understanding.
5. Pay Attention to Facial Expressions and Gestures
Even if the person isn’t showing a lot of expression, they are likely still reading yours. You can use nonverbal cues like smiling, and nodding, and use gestures to emphasize your words.
If you’re unsure how they’re feeling, ask questions gently rather than making assumptions. Help them express emotions in other ways, such as with facial movements, a thumbs-up, or eye contact. Using expressive body language supports better non-verbal communication, especially when speech is limited.
6. Encourage Use of Assistive Devices
Tools such as speech amplifiers, tablets with speech apps, or communication boards can make it easier to express needs. These assistive devices for Parkinson’s patients are especially helpful as speech challenges progress. An occupational or speech therapist can recommend the right tools based on individual needs. Supporting their use boosts confidence and keeps communication flowing, even during difficult moments.
7. Take Breaks if Needed
Sometimes conversations become tiring or frustrating for both parties. If you notice signs of fatigue or stress, suggest taking a short break and returning later. This helps avoid feelings of defeat and keeps communication positive. Short breaks also allow time to rest, refocus, and return to the conversation with a refreshed mindset.
8. Ask Yes/No Questions When Appropriate
Open-ended questions can be overwhelming. Try offering simple choices or yes/no questions when appropriate, for example, “Would you like to go outside?” This simplifies decision-making and encourages participation without pressure. Yes/no questions allow the person to respond quickly and feel included in conversations, even on difficult days.
9. Involve Speech Therapists When Needed
A speech-language pathologist is a valuable part of Parkinson’s care. They provide personalized strategies for improving clarity, breathing, and vocal strength. If your loved one is having difficulty speaking or being understood, professional guidance can make a big difference. A therapist can also suggest communication tips for Parkinson’s care tailored to your unique situation.
10. Focus on Connection, Not Perfection
Conversations don’t have to be flawless. Focus on listening, showing empathy, and creating a supportive environment. Learn how to talk to someone with Parkinson’s in a way that emphasizes understanding and companionship rather than perfect speech. The quality of the connection matters more than the words themselves.
Supporting Communication in Advanced Stages of Parkinson’s
For individuals in the later stages of Parkinson’s, verbal communication may become extremely limited. In these situations, non-verbal methods become essential in maintaining connection and understanding.
Try using simple hand signals, picture cards, or even pointing to objects or photos. Eye movements and facial cues, such as raising eyebrows or blinking, can be developed into consistent signals for basic needs like yes or no, pain, or help.
A communication journal can also be helpful. Keep it nearby to track patterns, behavior changes, or non-verbal preferences the person might not express out loud.
As a caregiver, it’s important to remain calm and reassuring. Speak slowly and clearly, even if the person cannot respond. They may still understand more than you realize.
A speech therapist or occupational therapist can help establish communication routines that match the individual’s abilities. These routines foster dignity and ensure their voice—spoken or not—is still heard.
Final Thoughts
These communication tips for Parkinson’s disease are designed to help both caregivers and loved ones navigate daily conversations with greater ease and compassion. Remember, it’s not just about the words, but it’s about the connection, the patience, and the presence you bring to each interaction.
Supporting someone with Parkinson’s involves more than physical care. Effective communication strategies for Parkinson’s also play a critical role in reducing frustration, improving emotional well-being, and maintaining strong, supportive relationships. With a little effort and understanding, your conversations can remain meaningful and empowering.
The smallest communication breakthroughs like a shared laugh, a nod of understanding, or a moment of eye contact can make the biggest emotional impact. Stay patient, stay present, and keep the lines open.
If you’re looking for additional support or communication tools for Parkinson’s care, don’t hesitate to reach out to professionals who can help tailor the right approach for your loved one’s unique needs.
